Acute valvular emergencies
Web link: Open online
Zotero link: Open in Zotero
Tags: cardiogenic shock, heart failure, Cardiology,
Abstract
Acute valvular emergencies represent an important cause of cardiogenic shock. However, their clinical presentation and initial diagnostic testing are often non-specific, resulting in delayed diagnosis. Moreover, metabolic disarray or haemodynamic instability may result in too great a risk for emergent surgery. This review will focus on the aetiology, clinical presentation, diagnostic findings, and treatment options for patients presenting with native acute left-sided valvular emergencies. In addition to surgery, options for medical therapy, mechanical circulatory support, and novel percutaneous interventions are discussed.
Notes
Annotations
(8/6/2022, 9:48:23 PM)
“In acute mitral and aortic valvular regurgitation, sudden rises in LV end-diastolic volumes lead to rapid elevations in LVEDP, left atrial (LA) pressure and pulmonary venous pressures with resultant pulmonary congestion (Figure 1). While there is some augmentation in total stroke volume due to the Frank–Starling mechanism, high regurgitant volumes result in decreased forward flow and a low effective cardiac output. This is compounded in acute aortic regurgitation (AR), wherein severely ↑LVEDP may cause premature closure of the mitral valve and diastolic mitral regurgitation (MR), resulting in further impairment of effective cardiac output and greater ↑ pulmonary venous pressures (Figure 2).5,6 Compensatory tachycardia is common to both acute valvular lesions, however, is often inadequate to preserve forward stroke volume and may be detrimental in those with a Type A aortic dissection or concomitant ischaemia. It is worth noting that acute mitral or aortic regurgitation is better tolerated in patients with pre-existing valvular regurgitation and normal LV function, compared with those with impaired systolic or diastolic LV function, ischaemia, or aortic dissection.” Go to annotation (Bernard et al., 2022, p. 1)
“While ‘classic’ (and eponymous) auscultatory findings associated with severe mitral and aortic valvular regurgitation are characteristic for chronic valvular regurgitation, findings in acute valvular regurgitation are different and often elusive (Figure 3).4 Notably, in up to 30% of patients with acute myocardial infarction and acute severe MR, no audible murmur is noted at all.” Go to annotation (Bernard et al., 2022, p. 2)
“important contributors to the delayed diagnosis of acute valvular regurgitation are (i) conflation of ‘classic’ physical examination findings in acute versus chronic valvular regurgitation and (ii) overestimation of the sensitivity of the physical examination in diagnosis.” Go to annotation (Bernard et al., 2022, p. 3)
“The application of colour Doppler is most likely to clue the clinician in to acute valvular regurgitation as the primary aetiology of decompensation. While large areas of flow convergence with a prominent vena contracta are typically seen, very severe lesions may lack turbulent flow owing to rapid equalization of chamber pressures. Eccentric jets should be well delineated to avoid underestimation of the degree of severity. Of note, quantitative measures for valvular regurgitation (e.g. effective regurgitant orifice area, regurgitant volume) should not be used given their decreased accuracy in the context of tachycardia and altered loading conditions secondary to cardiogenic shock.” Go to annotation (Bernard et al., 2022, p. 3)
“Continuous-wave Doppler profiles of acute MR will typically be
- densely echogenic,
- have a low peak velocity (< 5 m/s) and
- triangular in shape, reflecting rapid equalization of pressures between the LV and LA.
Analogously, continuous-wave Doppler profiles of acute AR will also be densely echogenic with a short pressure half-time and low-end diastolic velocity (reflecting rapid equalisation of aortic and LV pressures)” Go to annotation (Bernard et al., 2022, p. 3)
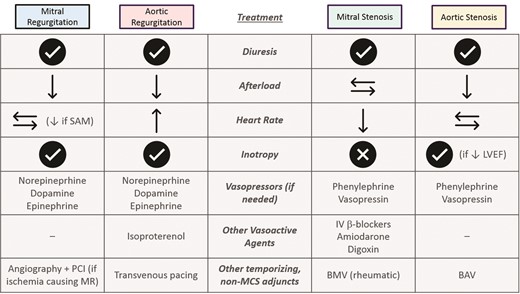
“Medical therapy for acute mitral and aortic regurgitation is limited and primarily focused on diuresis and afterload reduction (Figure 7). Reduction in systemic afterload promotes forward flow in both regurgitant lesions and therefore is a critical aspect of management. Similarly, diuretic therapy decreases overall pulmonary congestion. While heart rate has not been investigated to play a major role in the management of acute MR, ↓ heart rates are essential when the aetiology of severe MR is systolic anterior motion of the mitral valve. For patients with acute AR, ↑ heart rates shorten diastole and have been demonstrated to ↓ regurgitant volumes and ↑ stroke volume. For patients with low heart rates despite inotropic or chronotropic agents, transvenous pacing should be considered.” Go to annotation (Bernard et al., 2022, p. 5)
“Acute MR is well served by most of the available MCS options. IABP provides the least support but is the most widely and readily available and can rapidly decrease LV afterload. Similarly, Impella can result in direct LV unloading, however, should be used with caution (or avoided) in patients with papillary muscle rupture and may be difficult to position/ alarm frequently in the setting of normal LV size. TandemHeart and LAVA-ECMO are more technically challenging to insert given the need for transseptal puncture across the interatrial septum, however, have the benefits of direct LA unloading. Finally, VA-ECMO may be used, but is often done so in conjunction with TandemHeart, IABP or Impella to prevent pulmonary oedema from increased LV afterload.
On the other hand, acute AR represents either a relative or absolute contraindication to MCS, especially in the presence of concomitant aortic dissection. Diastolic balloon inflation of the IABP results in an increased regurgitant volume. The forward flow effects of the Impella are mitigated by severe AR, of which the latter may be worsened due to the device precluding aortic valve coaptation. AR and pulmonary oedema may be worsened in the setting of ↑ afterload with VA-ECMO. If MCS is absolutely necessary, TandemHeart or LAVA-ECMO could be considered due to concomitant LA unloading” Go to annotation (Bernard et al., 2022, p. 7)
“Patients with acute decompensation in the setting of severe valvular stenosis will present with dyspnoea due to a rapid rise in LA pressure ± LVEDP. Some patients will have cardiogenic shock depending on the precipitant and remainder of cardiac function. Other clinical symptoms may be present depending on the cause of deterioration” Go to annotation (Bernard et al., 2022, p. 7)